Understanding the Organ Donation Process: Donation After Brain Death (DBD) and Circulatory Death (DCD)
Most Americans support organ donation. But here’s a surprising fact: only about 1-2% of deaths in the U.S. clinically allow for organ donation. This is one reason for the scarcity of organs, which means sadly 16 people die waiting for a lifesaving transplant each day.
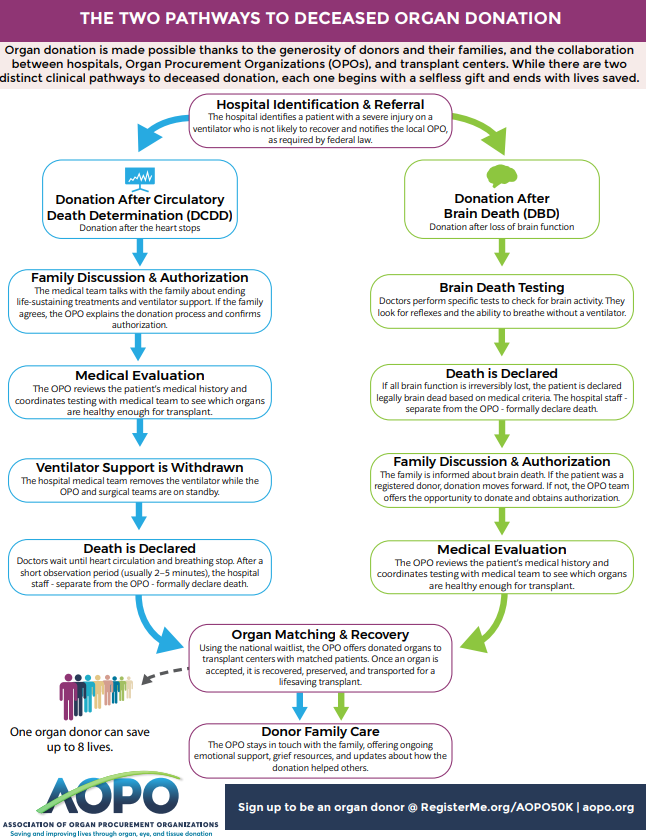
That’s because donation can only happen under very specific circumstances: donation after brain death (DBD) or through a process called donation after circulatory death (DCD).
While both pathways can save lives, they are different. And most importantly:
The patient is always deceased prior to surgery and recovery of organs.
Who Decides When Death Has Occurred?
In every donation scenario, the hospital – not the organ procurement organization (OPO) – determine when a patient has died.
Organizations like Network for Hope play no role in declaring death. This safeguard protects patients and upholds strict medical and ethical standards.
Two Pathways to Organ Donation
1. Brain Death
Brain death is death, medically and legally. According to the American Academy of Neurology, it occurs when there is catastrophic and irreversible loss of all brain function, including the brain stem.
Common causes include:
- Severe head trauma
- Stroke
- Medical conditions that cause the brain to swell and stop functioning
Even though a ventilator can keep the body’s organs working for a short time, the person has died.
Once brain death is confirmed by the hospital’s physicians (who are not part of the transplant or donation team), their time of death is documented.
If the patient is a registered donor, or if the family authorizes donation, the OPO can begin the donation process (including evaluating organs, contacting transplant centers, etc.) which can take several hours.
2. Donation After Circulatory Death (DCD)
DCD occurs when a patient has a severe injury or illness they cannot survive, but they are not brain dead.
They are dependent on a ventilator, and the hospital physicians and the family agree that further treatment will not change the grave prognosis.
Here’s how the process works:
Step 1: Medical decision to end life‑sustaining treatment
The patient’s hospital care team talk with the patient’s next of kin or family. They make the decision to remove the ventilator. The OPO is not involved in this decision.
Step 2: Authorization for donation
If the patient is a registered donor, the OPO honors that decision. If not, the legal decision‑maker is asked if they choose to authorize donation.
Step 3: Preparing for donation opportunity
The hospital continues to provide full comfort care while the OPO evaluates whether the patient’s organs are healthy enough for transplant. This evaluation and work to find potential matches can take several hours.
Step 4: Hospital removes the ventilator
The ventilator is removed in a planned, respectful setting – often in the operating room. The patient receives the same comfort care as someone who is not a donor.
Step 5: Declaration of death by Hospital
Once the heart stops and breathing ceases, hospital physicians wait at least five minutes to ensure it does not restart. Only then is death officially declared by the hospital physician, not the OPO.
Step 6: Organ recovery
After death is declared, the surgical team begins organ recovery. In DCD, kidneys, liver, lungs, and pancreas are the most commonly donated organs. Heart donation is sometimes possible but less common.
If the Heart Doesn’t Stop Right Away
In some cases, after the ventilator is removed, a patient’s heart may not stop for a longer period of time. If the patient does not die within the medical time frame (usually 90 minutes), organ donation cannot take place because the organs are no longer be viable for transplant.
At 90 minutes, the organ donation opportunity ends.
Although organ donation is not possible, the OPO family support team may remain available if the family wishes but their role is entirely to provide emotional support. The donation opportunity process has ended. The hospital team continues end‑of‑life care in the patient’s room or care facility.
Common Questions About DCD
Is the patient still alive when donation begins?
No. Organ recovery never starts until the patient is declared dead by the hospital’s physicians.
Can families still say goodbye?
Yes. Families have time for private goodbyes, moments of silence, honor walks, or other memorable moments before the donation process begins.
How is death declared?
After life support is removed, hospital physicians monitor the patient. Once the heart stops, they wait at least five minutes before officially declaring death.
Why Transparency Matters
Recent news stories have raised concerns about organ donation. These headlines are sensationalized and have caused some people to remove their names from the donor registry which only hurts those patients who are waiting for a transplant.
Learn more: How the Organ Donation Process Works – AOPO
factsaboutorgandonation.com